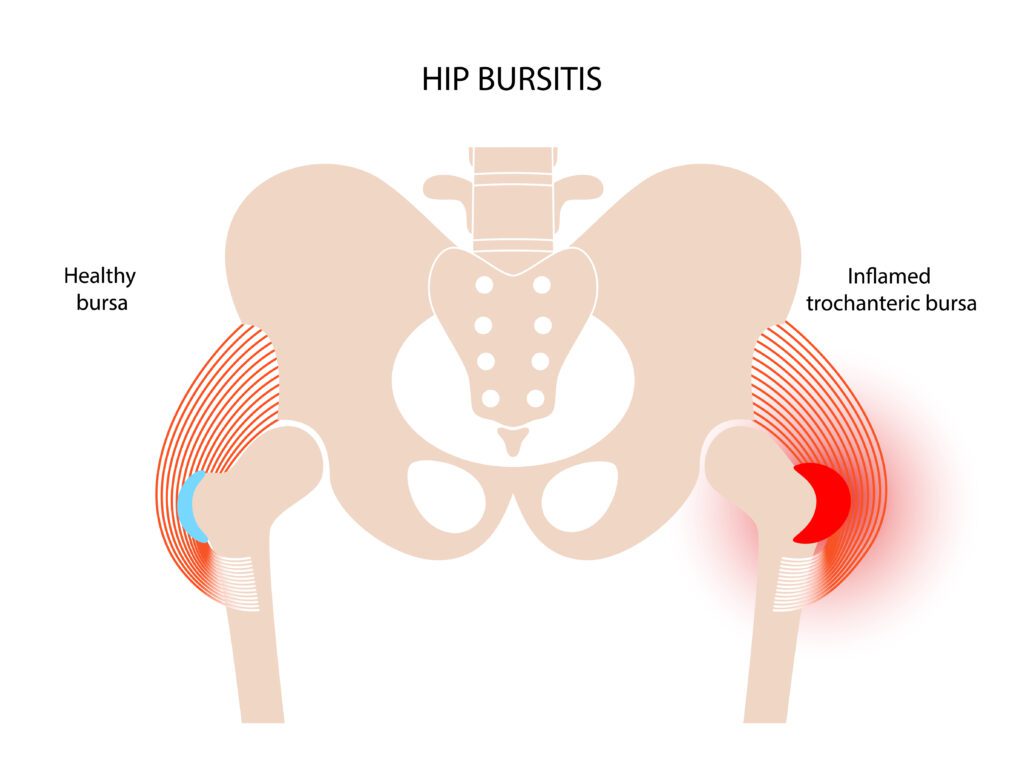
The more accurate name for this pain at the side of your hip is gluteal tendinopathy (+/- trochanteric bursitis, aka greater trochanteric pain syndrome). Trochanteric bursitis is inflammation of the trochanteric bursa which sits over the outside of the hip bone (trochanter). The bursa provides lubrication and cushioning to allow the muscles to flex and extend over the trochanter without damaging the muscles. It also cushions the tendon before the attachment of the gluteus medius and minimus muscles.
Occasionally, this bursa can become inflamed and clinically painful and tender – this is called trochanteric bursitis.
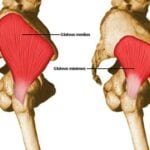
More often the lateral (outer) hip pain is caused by changes within the gluteal tendons (tendinopathy) which may secondarily inflame the bursa. Tendinopathy at the hip is an overuse of the gluteus medius muscle at its insertion to the trochanter. This results in a breakdown in the structure of the tendon and pain is produced when the muscle is used (such as with walking), this is most common in middle-aged women.
It can be difficult to distinguish between trochanteric bursitis and gluteus medius tendinopathy due to their proximity. Gluteus medius tendinopathys is usually tender to palpate (touch) just above the greater trochanter, your physiotherapist will be able to differentiate between the two conditions for you.
What does it feel like?
The symptoms are commonly an aching pain in the outside of the hip region that is exacerbated on walking, prolonged standing or sitting, lying on the same side, stair climbing, or running. In runners, it is commonly the result of overuse or overload rather than direct trauma. Although the classic symptom is lateral (outer) hip pain, it may radiate to the groin, or, in approximately one third of patients, pain will radiate into the lateral thigh.
What causes Trochanteric Bursitis?
This condition can arise after an injury (often resulting from a twisting motion or from overuse), but sometimes arises for no obviously definable cause. Some factors which may contribute to developing gluteal tendinopathy or trochanteric bursitis include:
- Overload of tendon- increased time on feet or standing with load all on one leg
- Leg length discrepancy (usually a difference of 3cm or more is clinically significant)
- Gluteal weakness often causing a “hip drop”
- Inappropriate foot wear
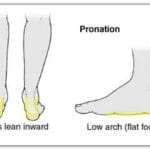
- Poor biomechanics – e.g. excessive pronation (or having flat feet)
- Weight gain
- Hormones eg perimenopause or post menopause
- Increase in exercise program – e.g. increasing distance, adding hills or stairs, increasing speed or change in terrain (grass vs sand vs road)
- Rheumatoid arthritis
These conditions lead to increased pressure of the muscles against the bursa and trochanter—with resultant inflammation of the bursa or overuse (tendinopathy) of the gluteus medius muscle.
What can I do to treat the problem?
- Ice – you can apply crushed ice wrapped in a wet cloth to the affected area for 10-15 minutes daily to help reduce the inflammation. Try to apply ice 2-3 times a day.
- Strength – Starting some gentle eccentric gluteal strengthening, your physio can help you with this.
- Stretch – Start some gluteal stretching e.g. pulling your knee up towards the opposite shoulder or put the ankle on opposite knee and pull up towards your chest.
- Correct any leg length difference – eg with a heel raise in your shoe, you physiotherapist or podiatrist can assist you with how high your heel raise should be.
When should I seek further help?
Gluteal tendinopathy and trochanteric bursitis do not usually resolve on its own as the contributing factors which lead to the condition occurring have not been dealt with. Start with some initial management of ice and rest from aggravating activities then see your physiotherapist to find out what other factors are contributing to your injury and what you can do to counteract them. A study published in the British Medical Journal was the first to show strong evidence that a load management and exercise program is more successful than a cortico-steroid injection – both long AND SHORT TERM. So ask your physiotherapist for an education and exercise program as first-line management for gluteal tendinopathy.
Reference:
Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial
https://www.bmj.com/content/361/bmj.k1662
.